The benefits of a steroid injection for Hay Fever
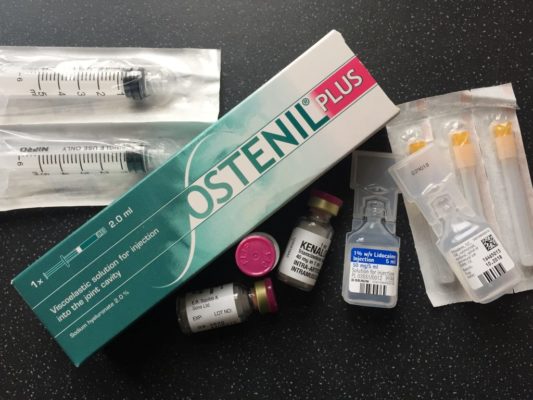
The injection is a single or double dose of corticosteroid (40mg / 80mg). This depends on the severity of symptoms or size of the person.
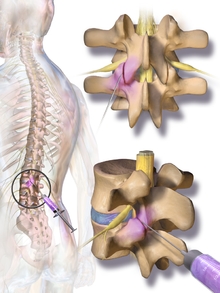
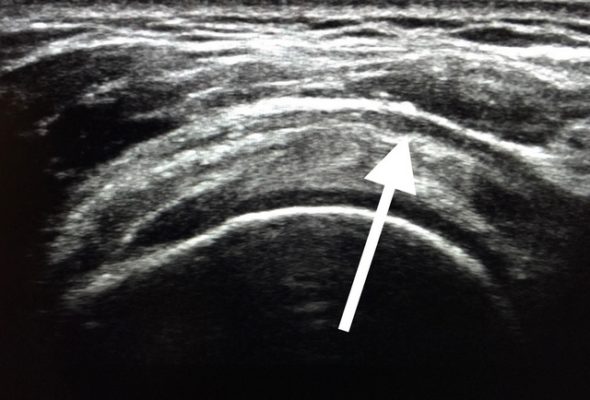
All hay-fever injections are administered in the gluteal muscle; this is confirmed by ultrasound to ensure optimal benefit.
Once administered the medication will suppress the excessive inflammatory response associated with hay fever. A single injection can provide relief for up to 3 months.
The total cost
The total cost of hay-fever treatment is £65 for 40mg / £95 for 80mg. There are no additional fees.
The risk
Under current Co-Vid 19 guidance patients must acknowledge that the use of steroids will decrease their immune response. This can make fighting the Co-Vid 19 virus more difficult. As a consequence, we strongly recommend you first try decongestants and minimise your exposure to pollen.
In keeping with current Co-Vid 19 guidance, any person who is shielding, high risk or presenting with Co-Vid symptoms is not eligible for injection.
Other exclusions include:
- Under 18 or over 70 (Co-Vid 19 protocol)
- If the person has or recently had cancer.
- Glaucoma
- Taking medication that could interfere with corticosteroid
- If your diabetes is unstable or have poorly controlled high blood pressure or other heart problems.
- Diagnosed with Osteoporosis.
Check you have got Hay Fever!
Please do not mistake hay fever symptoms for corona-virus or the other way round.
The symptoms of corona-virus typically include a high temperature and a new, continuous cough.
Hay fever does not typically cause a high temperature and most people with hay fever do not feel unwell. Their symptoms will also fluctuate with changes in the level of pollen.
Please phone 0114 2671901 or 01924 654068 to make your appointment.

Information on how coVID -19 is affecting clinical practice.
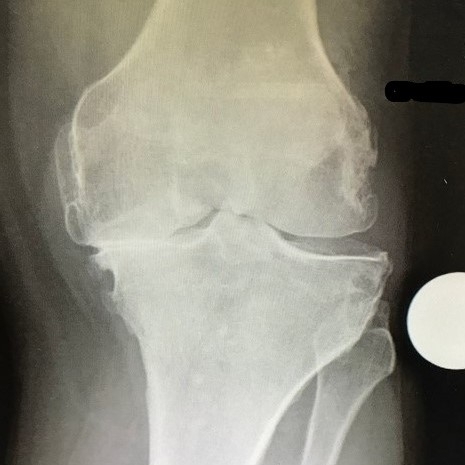
Ultrasound scans to help confirm your diagnosis will continue as normal. Remember, there are lots of changes that can be made to manage your problem once diagnosis is established.
What about the use of steroid injections
- Over the age of 70 years.
- Any immunosuppressant disease; such as Lupus, Inflammatory Bowel Disease and Type 1 diabetes.
- People with breathing problems such as Chronic Obstructive Pulmonary Disease (COPD) or asthma.
- And anyone with cardiac problems such as hypertension (high blood pressure) or angina.
Please Note: There are diseases and pathology that prevent good health irrespective of an individuals actions. The advice in this blog is not a substitute for medical opinion. Always consult your healthcare professional for specific advice on your personal condition. But please remember, best health irrespective of condition will always be optimised if your chemistry is made as good as possible.